As my title says, waking up is hard to do!
So how did I wake up?
Like Bugs Bunny coming out of his ether stupor…that’s how…
Having just come off of six years of schooling, the strongest skill I possessed was my tenacity for research. So when COVID was hitting the scene abroad, I was trying to figure out everything I could about what type of virus this was, how it was being transmitted, and how it could be treated. I cruised the usual places healthcare workers do for information on novel viruses and infection control: the WHO and the CDC. At first I was looking for clues on transmission.
Here’s where I hit the first red flag. No one was willing to definitively put in writing how this virus was transmitted. It was clear that the Chinese were wearing all of our generously donated PPE, but they were also wearing high tech respirator suits. That struck me as a strong signal this was an airborne virus, but no matter where I looked, I couldn’t find it in writing that this was an airborne virus. What I was seeing, however, were non-stop reports about contact transmission, in particular fomite transmission.
Here are just a few examples:
Here is a link to an article in Nature that nicely summarizes the entire fomite evolution: COVID-19 rarely spreads through surfaces. So why are we still deep cleaning?
https://www.nature.com/articles/d41586-021-00251-4
I went from being a regular OCD nurse about cleaning surface areas and washing my hands, to being an OCD nurse on steroids! I found myself wiping down surfaces in my home, cleaning my groceries, treating the pizza delivery guy like a culture swab, and generally tormenting my husband and children on transmission based precautions.
At the same time I was wiping shit down, I was researching the shit out of anything COVID I could get my hands on, as well as anything that might help with the symptoms of COVID. One of my close friends at that time was an NP working in a teaching hospital. She and I texted frequently. She was my eyes and ears on the front line, and I was her research assistant reading and sharing research that she just didn’t have the time to do. I had saved our texting thread, and noticed our first correspondence was March 25, 2020. This was right around the time I received those three requests to work.
I asked my friend how she was doing, and how it was going inside the hospital. She confirmed to me that the patients she was seeing were both old and young (50’s). She commented that the patients “go from fine to intubated in hours.” She also told me this day that, “They are responding to hydroxychloroquine and zithro” (azithromycin). When I asked her why the patients were crashing so fast she responded, “They crash quickly because we can’t do any intermediate interventions we can’t use nebulizers we can’t use steroids we can’t use high flow or BiPAP so they go from 6L of oxygen nasal cannula to intubation we don’t wait.”
This information was pretty surprising to me, and another red flag. Why wouldn’t they immediately intervene on patients in trouble? I asked my friend this exact question, I asked, “Are you restricted on Nebs for risk of aerosolizing everyone?” She responded, “Yes And hv to intubate in neg pressure too and can’t bag.” Let’s think about that for a moment. The patient comes into the hospital with difficulty breathing. Our usual protocols are to give steroids, bronchodilators such as albuterol via a nebulizer, and oxygen. If the patient decompensated, they would be intubated and placed on a ventilator, however my friend is saying that the patient had to be in a negative pressure room first in order for medical staff to intubate! You must understand prior to COVID there were about ONE Negative pressure room per critical care unit or medical floor. Post COVID we heard of engineers converting non-negative pressure rooms into negative pressure rooms, and/or using HEPA air purifiers, or HVAC air exchange increases.
For those of you unfamiliar with negative pressure here is a quick video to explain.
One thing nurses are known for is having to make straw into gold. That’s usually related to staffing issues, however, we are a creative bunch, and learn from our experience, and collaborative skills to figure things out, or get things done. When my friend explained to me they couldn’t intubate or give nebulizers unless they were in negative pressure rooms I thought immediately of the croup tent. Now, I never worked in pediatrics, but I did remember my pediatric rotation as a student, and thought why not just give the adults their nebulizers in a croup tent and reduce the amount of aerosolization worry? My friend who was unfamiliar with the croup tent, but caught on quickly with the image I sent her, loved the idea, and introduced it to the Pulmonologist. My idea was to assist with early treatment, and buy time to intubation. Remember we are still texting all this on that same March day….those pesky 12 hour shifts. I received a text back that morning saying, “He said he thinks it still aerosolizes i read that when its opened it mixes with room air. I think its a good alternative though if we hv nothing else.”
Fast forward to April 10, 2020 I received this text from my friend, “OMG! They are using a tent!!!! I mentioned it to my icu doc and he said no now they are using it!!!” I was so happy for the patients, but I was also so confused as to why a simple idea took so long to implement? Was it because a nurse thought of it?
On April 12, 2020 I sent my friend an interesting article I had come across during my daily research ritual. It was titled, Nebulized heparin and N-acetylcysteine for smoke inhalation injury: A case report , which she said she would read. On April 13, 2020 she texted me, “I'm giving this article to our pulmonologist in charge of the covids!!! The problem I think would be we aren’t using nebs.” I explained to her how I came about finding the article, and my relationship with NAC as a CCU nurse and how we gave nebulized NAC for mucous management of vented patients, and orally to pre-cath lab patients to protect the patient’s kidneys from the dye used during the angiogram. Then I texted, “…and I know you guys are seeing a lot of renal failure is that due to micro embolism, organ failure? Just thinking…” What I wasn’t thinking about was the lethal renal toxicity of Remdesivir because it hadn’t been approved for EUA yet. (That happened in May 2020.) Patient’s were suffering acute kidney injury due to hypovolemia and dehydration (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7546258/).
My next text, in retrospect, surprised me the most, because I couldn’t believe what I sent, when I sent it. I literally texted her this:
I can honestly say at the time I had absolutely NO idea who Dr. Paul Marik was. What I did know was that someone had put out a protocol, something that could possibly help, and I was spreading the good news!
Then I get this text on April 18, 2020, “Just speaking with a doc from brooklyn they are all dying from clots venous and arterial! I gave the the smoke inhalation article to our pulmonologist.” I asked, “D-dimers elevated on most?” She replied, “Yes!” then texted, “Both pulmonologists liked the idea lets see what happens.” I was pretty excited to see collaboration. We casually texted back and forth and on April 24, 2020 I asked her how she was doing. She responded, “Good tired doing 9 12 hr shifts in 12 days…” These were long hours, and long days, and long weeks!
On May 6th I received a text from my friend asking me to look for more evidence on the nebulized heparin and mucomyst. She was hoping to convince the head of research to try it in a study. I have no texting thread that follows this up. We text casually back and forth for a few months after that, and then on July 23, 2020 I asked, “Are you using budesonide nebulizer for mild to severe symptomatic COVID? I’m reading good things.” To which she replied, “Yes.” I asked her about effectiveness, but I never received a response to that text.
The day after Christmas, 12/26/2020, I sent out the FLCCC protocol, and I asked her, “…Are you guys prescribing ivermectin? If so what are you seeing? I’ve been researching this extensively.” Her response, “No Ive heard about it too…steroids are what’s helping…I think they should give steroids right off the bat but they wait.” I explained how Dr. Kory from the FLCCC were the same people who advocated for early steroid use are now advocating for ivermectin. And then she tells me she is leaving the hospital…and that was the end…
….the end of my inside scoop, but not the end of my story. To be clear, during the summer of 2020 I was working two jobs, my university job helping students who were behind from the spring lockdowns make up clinical hours, and my hospital position in the PACU, helping my unit catch up on all the surgeries that had been cancelled in the spring. My free time was spent researching.
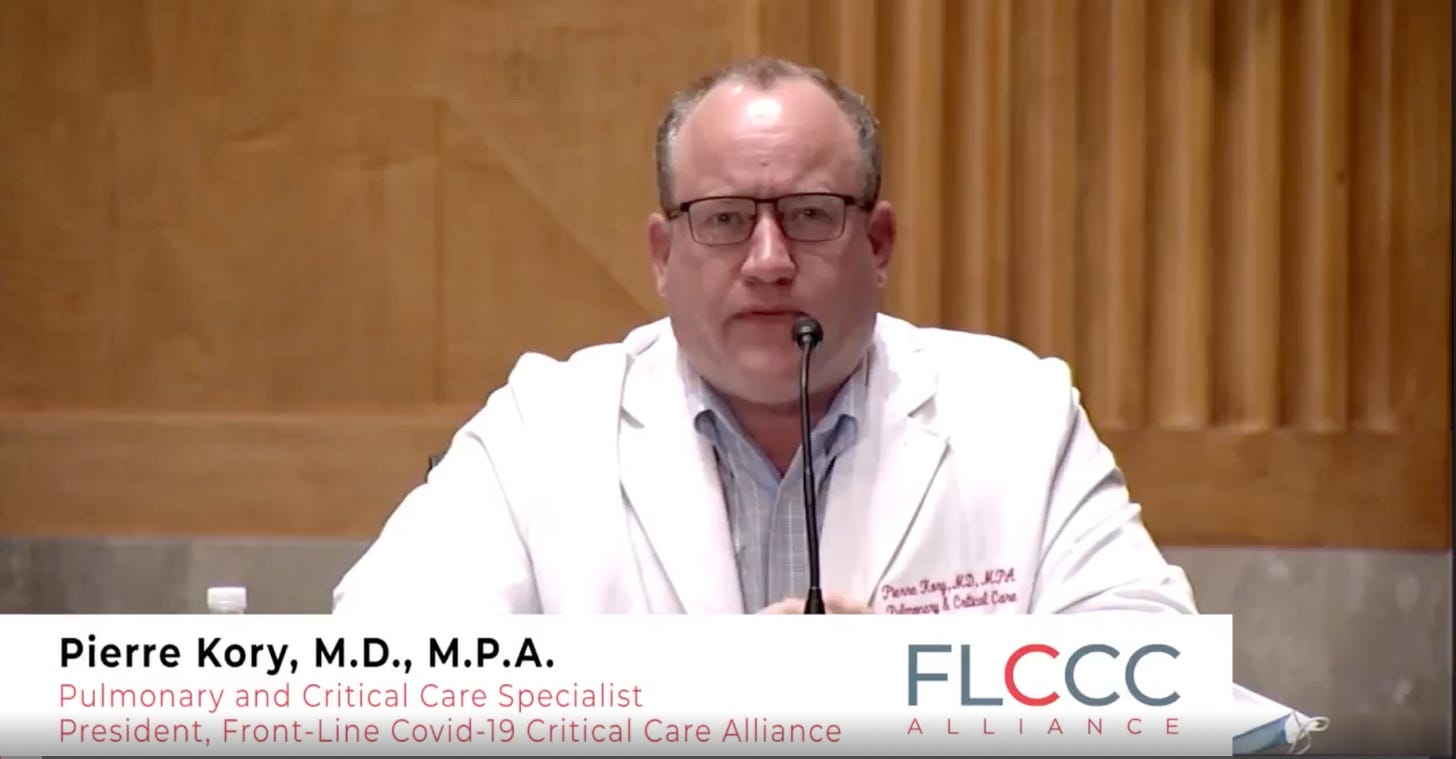
My true epiphany, the thing that began my journey down what some would call a rabbit hole, what I would call an awakening, came when I discovered Dr. Kory’s Senate Committee on Homeland Security and Governmental Affairs testimony video from December 8, 2020 hearing on “Early Outpatient Treatment: An Essential Part of a COVID-19 Solution”
The first time I heard Dr. Kory’s passionate testimony, I felt as if I knew this guy. He was an ICU intensivist, and I was a critical care nurse. His mannerisms, passion, and data driven presentation reminded me of other intensivists and critical care attendings I had worked alongside during my 34 year career. Nothing he said struck me as mis/disinformation. Now here is what separates the critical thinkers from vacuous fools…I didn’t just swoon and say, “Yes Doctor.” I listened, I was excited about this drug I had never heard of, I was hopeful for the patients, and I was careful to research what he was saying.
I immediately began researching everything I could about Ivermectin, the drug, the history, the pathopharmacology, the safety record, the adverse effects, it’s interaction with other drugs, you name it. I also began looking into Dr. Kory, which is how I came across his FLCCC Alliance, and his first video from May 6, 2020 testifying about the need for early steroid use in COVID-19 patients. I was really hopeful that Ivermectin was going to be a game changer for the management of COVID-19…really hopeful!
Reality is a bitch slap. It strikes you red on the cheek, shakes you like a rag doll, and drags you through the mud. Ivermectin was now in the same scope site cross hairs as hydroxychloroquine was, and it was clear my hope was in check. Ivermectin wasn’t going to be the next big thing, it was going to be the next big thing to destroy, and you could pretty much blame Joe Rogan for that, and those damned horses (and every major news network, TV doctor, and opinionated blue-haired leftist).
Because I love JP Sears so much I’m going to let him explain…
To be continued…







I reside in India and we faced the brunt of many bad policies during our Delta wave in mid-2021.
I also wrote about it here:
https://disinformationchronicle.substack.com/p/reporters-expose-pfizer-misinformation/comment/4001337
Although, I am now getting some clues that things were not as bad as they were portrayed in the media even here, which is good.
This article also reminded me of something I asked recently on Twitter. EVEN IF Covid19 was as bad as people said, given it comes and goes in waves, what EXACTLY does the medical community do during the troughs? Why didn’t the Doctors who were neutral on the utility of early treatment drugs, spend some time researching them during these troughs?
https://twitter.com/aravindmc/status/1526962828875210752
[ In case someone finds my account is suspended: I make a lot of snarky comments on Twitter - just to irritate the people who keep calling IVM as horse-dewormer, usually- and I also keep asking questions about vaccine injuries. I am sure I am going to be kicked out shortly :-) ]
Your article is a good example of someone during research during the trough, although your reason seems to be quite different. But I am still not sure why we did not see more of it from the frontline doctors and nurses?
Thank you for writing this and I look forward to reading your future articles. In a future article, can you also touch on why more nurses did not speak up, and maybe speak up a bit earlier? Was it just mostly out of fear of losing their jobs? Was it also genuine confusion about the disease itself? Were there any other factors that the outside world could not see?