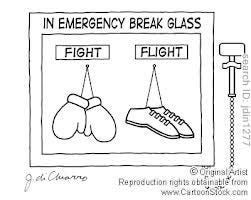
Like I said from Part I of this series, I was primed for fear. Fear is a great motivator or a great inhibitor. Our bodies know this and secrete hormones in times of danger to help us with our fight or flight response. There’s a little thing in our brain known as the amygdala. This is the emotional receiver of the brain that when activated in a stressful situation, sends out an SOS to the hypothalamus. The hypothalamus, or command center of our brain, assists in activating our fight or flight response by activating the sympathetic nervous system. This part of our autonomic nervous system sends signals over nerve pathways to our Adrenal glands (the glands that sit on top of each kidney). These glands then respond by pumping epinephrine into our bloodstreams aka adrenaline, which then allows us to run like hell, or fight for our lives. Our hearts beat faster, our blood vessels constrict to increase the pressure inside to push blood to our vital organs (heart, lung, brain), our bronchioles dilate inside our lungs allowing for more oxygen delivery to our brain, and our senses sharpen. Blood sugar and fats are released as a result of the the epinephrine release, increasing our energy.
The second part of this flight or fight system is the release of cortisol from the adrenal glands, stimulated by the hypothalamus’ continued response to the stressful event. In technical terms the hypothalamus releases corticotropin-releasing hormone (CRH), which travels to the pituitary gland (also in the brain), which releases adrenocorticotropic hormone (ACTH), which signals the adrenals to release cortisol, which keeps us up and running during that stressful event. When the threat has resolved, the second part of the autonomic nervous system, the parasympathetic nervous system takes over to slow everything down, and bring that stress response in for a landing. (https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response)
This is a great system, however it has one fault, that is we can turn this on for a real threatening, harmful crises, but we can also turn this system on for a perceived stressful crises such as a deadline at work, a school paper that’s due, worrying about a sick child, or living in constant fear of a virus. And when we turn this system on and don’t turn it off, we are at risk for chronic health problems both physical and psychological.
For the past two and half years it feels as if the world turned this system on over fear of a virus, and only those that woke up, (or the lucky ones who were awake from the get go), have turned it off. What remains, is obvious to most people, that those still living in this state of fear are suffering from a chronic psychological issue, that may have been present pre-COVID, and was exacerbated, or may have developed during COVID. Either way it remains ongoing for a certain percentage of the population.
As I described in Part I, I have lived through many viruses, and taken care of many patients throughout my career. I mostly had those adrenaline driving moments when my patient’s lives were in jeopardy or sometimes my own - think cardiac arrest patients, respiratory arrest patients, pediatric patients with worried moms at the bedside, crazy running down the hall naked patients, patient who told me they got a knife through security and spent time in prison, patient who threw a telephone at me, patient who fell on the floor…you get the picture. But not once did I have this adrenaline rush when someone said to me, your patient has HIV, or your patient has Legionnaires disease, or your patient has influenza, or your patient has multi-drug resistant tuberculosis, or pan-resistant Acinetobacter baumannii, or C. Difficile, or methicillin-resistant staph. aureus (MRSA), or vancomycin-resistant enterococci (VRE), or Carbapenem-resistant enterobacteralus (CRE). I even had a nurse friend of mine whose patient had Leprosy, and we laughed about it, and joked “only in NY.”
So what happened to me in the spring of 2020 took me by surprise more than I’d like to admit, because in January of 2020 as reports of a novel virus were emerging from a place called Wuhan China I was still in a pretty calm place of thinking here’s another coronavirus somewhere else, and not something I need to worry about. That quickly changed when in February of 2020 the reports and images started coming out of Lombardy Italy of the devastating effects of this new coronavirus epidemic, including the devastating toll on healthcare workers. By this time the U.S. was also seeing coronavirus cases and death, and on March 1, 2020 the first COVID-19 case was diagnosed in my great state of NY. Something unfamiliar started creeping up my spine, raising my pulse, and knotting up my stomach…
In 2013 I decided to go back to school. My hospital was seeking Magnet Status . I knew if I didn’t go back to school, my associate degree in nursing (though grandfather-able), would be obsolete, and there would be no room for professional growth. I completed my RN to BSN online while raising my family, and working part-time. Once completed, I realized that as much as I loved being at the bedside taking care of patients, I didn’t want to have to be there as an older nurse. I decided to continue on in my education and perused my master’s degree in nursing education. I had always volunteered to precept new nurses, learn the most challenging equipment, function as charge nurse, work on unit education projects and so on. Nursing education was a natural transition. I graduated in the spring of 2019, and by the fall of 2019 I had landed my dream teaching job at a local university working side by side with the students teaching them their fundamental skills in the simulation lab. I continued to work per-diem at my local community hospital, because you could take the nurse away from the bedside, but you couldn’t take the bedside away from the nurse. I loved taking care of patients, and I loved being able to bring my bedside experience to my young nursing students.
As my second semester progressed, we were all incredibly aware of the murmurings out of Wuhan. I had just completed quite a few shifts over the winter break that January of 2020, and my radar was up. College campuses, however are a different animal. Most of the nurses I worked with no longer worked at the bedside. The higher the degree you had, the further from the bedside you were. As the COVID anxiety seeped in through the media reports, it was becoming palpable at the office. When that first NY patient was announced it was pretty obvious we weren’t too far behind Italy.
On March 7, 2020 our former, disgraced, NY Governor Andrew Cuomo declared a state of emergency, and on March 10th he ordered a containment zone in New Rochelle where the first patient diagnosed with COVID-19 was from. On March 11th our University had closed the campus and switched to remote online learning, and by March 14th NY had seen its first two COVID deaths. This shit was getting real…fast! My small university crew that I worked with were quick to rise to the challenge of remote learning. For one thing, we worked in a simulation lab. We were not tech shy. For another thing, I had just come off of six years of online learning, to say I was comfortable in this format was an understatement. So the show went on-line, and as we worked to complete the semester, my hospital colleagues were working to save lives.
By the end of March 2020 the ICU I used to work in was filling up fast, and the overflow of critical patients were moving to PACU (my unit) as a temporary ICU. This was still a very busy time for me at the university, but I expected the hospital would be looking for me. From the end of March to the end of May was considered to be the first wave of COVID-19. This is where the ground was laid for fear and panic. This is where, for the first time in my career, I feared a virus. This is where, for the first time in my career, I felt ashamed for not being in the trenches with my coworkers, but instead worked from home hosting a new online teaching platform called zoom.
I bought into the fear hook line and sinker like the rest of the world. I believed every word coming out of my TV. I am ashamed to admit it, but I posted things on my Facebook page that said, “6 ft. apart or 6ft under.” I was the super Karen washing my groceries, and using gloves to handle the pizza delivery box. I worried for my 79 year old mother, and my husband who both had comorbidities. I had become something and someone that I didn’t recognize. In retrospect, I am mortified. However, I am being totally honest and transparent because this is my history, and I cannot whitewash it.
I also worried my phone would be ringing off the hook with the hospital looking for me to come in and work. But this didn’t happen. All in all I was asked three times to come into the hospital during the first wave of COVID. The first request, at the beginning, was sent to me and my best friend to help out in the ICU. As I debated going in with my husband, my best friend agreed to take the shift. The next two calls to come in coincided with my full-time university job, and I was unable. After that I wasn’t asked to come in again until the end of the first wave, when our PACU was reopening for elective cases. At first I thought it was weird no one called me, I also thought maybe it was because they knew I was working full-time somewhere else. I ended up calling my other coworkers, who like me, worked per-diem, and they said they weren’t being called in either.
This was such a red flag for me.
To be continued…





Wow!! Yes… that red flag!! No calls to come in.. can’t wait for Part 3!